HEEL BONE (calcANEAL) fractureS
By: Robert H. Sheinberg,
D.P.M., D.A.B.F.A.S., F.A.C.F.A.S.

What is the calcaneus?
Answer: It is the heel bone that has a hard outer
shell and soft inside. The top of the bone has cartilage that assists
the bones in the foot in moving.

How do injuries occur?
Answer: Injuries usually occur from falls from a
height or jumping off of a high object (i.e. table, roof or ladder).
What happens to the bone when it gets injured?
Answer: It usually shatters into multiple pieces
(comminution). The bone shortens in height and increases in width.
What injuries are associated with these fractures?
Answer: Injuries may occur concurrently to the wrist
and lower back.
What should be done immediately after the injury?
Answer: The immediate application of ice and
compression will keep down some of the swelling. Strict
nonweightbearing with crutches is extremely important. Immediate care
is necessary from your physician.
How is the injury evaluated?
Answer: Complete history and physical exam of the
injury is performed. X-rays are taken to evaluate the fracture
itself. In most cases a CT scan is necessary to evaluate the joint
surfaces and determine what the best surgical procedure to be performed
is. Injuries to other areas including the wrist and spine are also
evaluated.
Will the foot be placed in a cast or will surgery be necessary?
Answer: Nondisplaced fractures may be casted.
The patient is put on crutches for six weeks. Displaced fractures will
usually require surgery.
How is it corrected?
Answer: The bone fragments are usually displaced or
out of their normal alignment. These fragments need to be put back
into their original position and held with pins, screws and plates.
Does surgery require hospitalization?
Answer: The procedure is usually performed in an
outpatient setting. If there are other conditions associated with the
fracture or medical conditions co-exist, hospitalization may be needed.
What possible postoperative care may be needed to insure good
recovery?
Answer: Patients will remain nonweightbearing for six
to twelve weeks.
When could a person return to work or sports following these
injuries?
Answer: Sedentary jobs can resume after one to three
weeks. Work requiring extensive weightbearing may take six to twelve
months. If the bone injury is severe, a change in a person’s job may
be needed. Sports modifications will also be necessary.
Will there be work restrictions?
Answer: Sedentary jobs will provide little problem
for patients with calcaneal fractures. Work restrictions will be
necessary for the person who has to weightbear. Walking long distances
or standing for a period of time will adversely affect the foot. These
restrictions may be in place for up to one year. In some cases these
restrictions may be permanent.
Will there be activity restrictions?
Answer: Activities that require walking long
distances or running will be limited. Return to some sports may take a
year or more. In some cases, where the fracture is severe, activities
that do require any type of lengthy weightbearing will no longer be
allowed. Sports that require side to side motion (i.e. tennis) may be
affected.
Will there be an impairment rating given to an employee injured at
work?
Answer: These injuries are associated with an
impairment rating. The injury does lead to arthritis in an important
joint in the foot. Additionally, stiffness is always seen in this
joint (subtalar), and the ankle joint may also be affected.
What are some long-term problems that may develop?
Answer: The most common problem that will develop is
osteoarthritis in the joint that connects the foot to the ankle. This
joint is responsible for assisting people to move from side to side.
It is called the subtalar joint. In addition, this joint helps the
body absorb shock when the foot hits the ground. Other problems that
may develop include tendon and nerve dysfunction. Difficulty with
wearing shoes may also be present, as the heel bone may be widened.
There is often discomfort on the bottom of the heel, as the fat pad under
the heel gets injured as well.
What is the long-term prognosis?
Answer: The injury to the cartilage is often
overlooked with these types of fractures. Once the cartilage has been
broken, osteoarthritis will often develop. The more pieces that are
broken. the worse the prognosis. Occasionally a two or three part
fracture is seen. This is where the bone has been fractured in only
two or three pieces. It is easier to put this bone together and the
prognosis is better. Full return to sports and activities performed
prior to the injury will be somewhat limited.
Will further surgery be necessary in the future?
Answer: If the bone has widened during the initial
injury causing tendon and nerve problems, a piece of bone may be taken off
the outer wall of the heel to reduce the bulkiness. If the joint
develops osteoarthritis that is mild, arthroscopic surgery may be performed
to clean out the joint. If the arthritis is severe, a fusion of the
joint to prevent any type of motion will be needed. This will
eliminate the pain and allow normal mobility. Occasionally, the
hardware that is placed in the fracture site will become an irritant and
this may also be removed. If the ankle has been affected by this
fracture an arthroscopic procedure to remove any abnormal tissue may be
warranted.
How will a fusion affect my foot and will the fusion cause problems in
other areas?
Answer: A fusion to the injured bone and joint will
virtually eliminate pain in that region. Fusion to the subtalar joint
will cause the ankle joint to work harder in allowing the foot to ambulate
as normal as possible. The ankle may become affected later, as
osteoarthritis may develop from overuse. Sometimes the osteoarthritis
is completely asymptomatic. Once a fusion is performed in the foot the
person will be able to resume work with little or no restrictions unless the
work or activity requires a lot of side-to-side movement. Pain will be
eliminated. It is by far the best procedure that we could perform in
this joint, as our ability to do other procedures and provide relief is
limited. If the ankle does become painful, arthroscopic surgery may
help to eliminate the pain.
What are the different types of calcaneal fractures?
1. Extra-articular
2. Intra-articular
3. Stress fracture
1. Extra-articular


Pre and Postop Minimally Invasive Percutaneous Fixation Displaced Extra-Articular calcaneus fracture in RA patient


X-ray of avulsion fracture of the calcaneus where the Achilles pulls off a fragment of the heel bone (below left). Another example of an extra-articular fracture of the calaneus is the tongue type fracture show in an adolescent (bottom right).


If secondary fracture line travels parallel with the plantar aspect of the foot, exiting at the posterior border of the calcaneus, a tongue fracture will develop.
- Secondary fracture line extends posteriorly from superior part of primary fracture line (at crucial angle), creating 1 single posterior, superior, & lateral fragment.
- Hence, the coronal fracture occurs posterior to the tuberosity.
Includes:
- Sustenacular fragment: - contains medial aspect of posterior articlar fragment.
- Tongue fragment: contains tuberosity & lateral aspect of posterior articular fragment.
- Inferior portion of body of the calcaneus.
- Fragmentation of the lateral wall is often mild.
- Comminution anterior to the Angle of Gissane will often be severe.
- Tongue fracture fragment will include portion of achilles tendon.
- With displacement of tongue fragment there will be excessive tension on the posterior skin which can lead to necrosis.
Treatment:
- ORIF fracture fragment.
- Removal of fracture fragment and advancement of Achilles to calcaneus.

Series of Intraop Pics of an Achilles rupture with part of posterior calcaneus still attached. This was a 17-year-old competitive cheerleader who jumped and injured her heel.
The Achilles torn off of the back of the calcaneus and a portion of the heel is still attached to the Achilles. The back of the heel bone is the rounded yellowish bone at the bottom of the incision site.

Nonabsorbable suture has been weaved through the Achilles to repair it back to the back of the calcaneus

A trough is made in the calcaneus due allow the tendon to have ingrowth at its reattachment site in the posterior heel.

The suture from the Achilles is placed through two small drill holes in the trough and out the bottom of the heel bone.


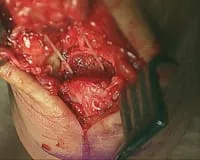
The Achilles is tensioned down into the trough and reattached to the calcaneus


2. Intra-articular
Intra-articular fractures are called as such because the fracture lines enter and can disrupt the articular joint surface. In the case of calcaneal intra-articular fractures the subtalar joint is the one that is post likely affected by this phenomenon. When the joint surface is affected is a priority to assure that the joint surface is minimally affected and if it is disrupted the priority then become to re-establish the joint surface usually with surgical intervention to assure the best outcomes.





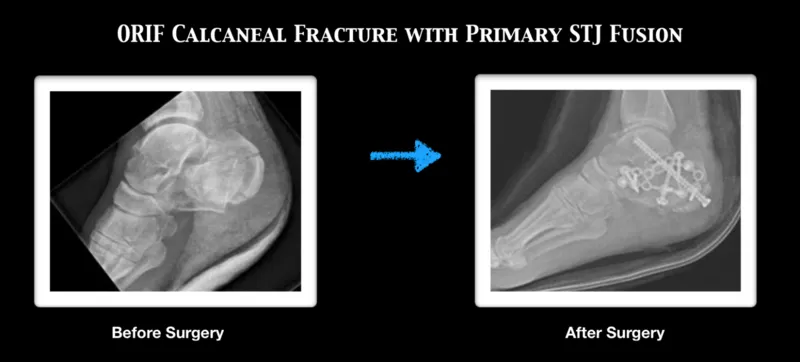

This is a picture before open reduction internal fixation (ORIF) of a displaced intra-articular calcaneal fracture.

These are pictures after plate and screw fixation of the above fracture. In these views, the joint surface has been reduced and then reestablished.


These are two pictures of an intra-articular calcaneal fracture with joint depression and displacement prior to repair.


The following two pictures are after repair and reestiablishment of the depressed joint back to normal alignment (ORIF calcaneal fracture).


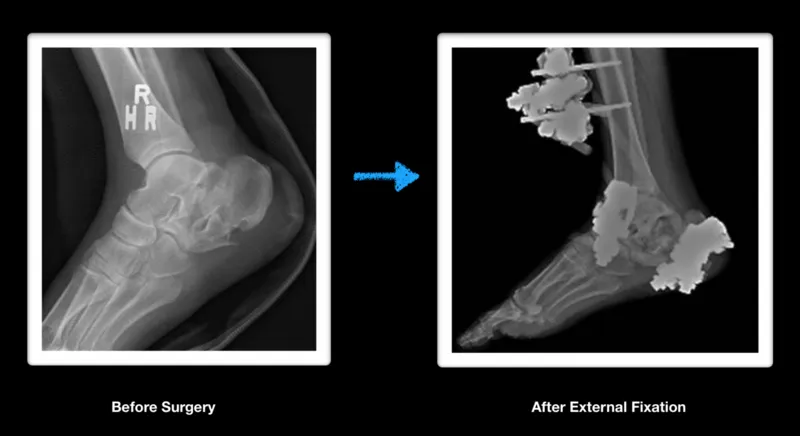
Pre and Postop calcaneal fracture









CT scans of intra-articular calcaneus fracture



3. Stress fracture
Stress fractures of the heel are uncommon in children. However, may be seen in young teenagers. A microfracture that usually occurs in the heel is due to abnormal stress that has been placed upon it. The most common presentation is a young athlete who presents with a sudden alteration in their training regimen, (i.e., more sprinting, increased mileage or increased training intensity) that develops global pain around the heel. Swelling may or may not be seen with this problem. This type of injury is more common in women, especially those with menstrual irregularities and lower calcium intake.
CAUSES:
- Stress fractures are overuse injuries that cause stress to the bone that exceeds the bone’s ability to repair itself.
- Repetitive stress to the bone over a short period of time, especially in an unconditioned athlete.
- Usually seen at the beginning of a sports season.
- Structural abnormalities of the heel bone (cavus or high arch foot) may predispose the patient to this problem.
SYMPTOMS:
- Diffuse tenderness to the heel bone upon grasping the heel. More of the tenderness is to the outside than inside of the heel bone.
- Occasionally seen with low-grade swelling on the outside of the heel.
- Pain may be minimal in the morning but as the day goes on pain gets worse, causing difficulty walking.
- Inability to participate in any type of sporting activity due to pain.
X-RAYS:
- Usually negative for stress fractures of the heel. MRIs and bone scans are rarely necessary as the diagnosis of stress fractures is made by a good clinical examination.
TREATMENT:
- Rest from the activity precipitating the problem. Cross training activities that do not stress or overload the bones (example: swimming, cycling, Stairmaster).
- Immobilizing the extremity in a removable boot usually lessens the pain immediately and allows ambulation.
- If unresponsive to immobilization in a removable boot, utilizing a fiberglass cast will immediately allow healing of the bone to take place.
- A change to a softer running athletic surface and the use of cushion shock absorbing custom molded orthotics.
- In females with menstrual irregularities, follow up with a physician is imperative.
- calcium and vitamin D supplementation.
PROGNOSIS:
Prognosis of stress fractures to the heel (calcaneus) is usually
excellent. The condition usually takes between 4 and 8 weeks to
heal. In the competitive athlete it usually takes 6-8 weeks before
activity can begin. Predisposing factors must be identified and
treated appropriately. Long-term recurrence is rare.
MRI imaging is excellent for diagnosing stress fractures. A T1 weighted image will show normal bone in a white color and edema and/or fracture lines in gray to black color (below left). T2 weighted imaged are the opposite and will show bone black and any fluid like swelling within the bone or throught a fracture as white (below right).