CAUSES OF OUT-TOE
By: Robert H. Sheinberg, D.P.M., D.A.B.F.A.S.,
F.A.C.F.A.S.



A.
FEMORAL RETROVERSION
Femoral retroversion is a positional deformity caused by contracture of the
external rotator muscles of the hip. It becomes apparent as the child
starts to stand or cruise between 6 and 9 months.
CAUSE:
- Tightness of the muscles of the hip that cause the hip to rotate excessively to the outside.
- Primarily caused by in utero position.
- Rarely caused by bone deformity in which there is an actual external twist of the lower portion of the upper leg bone (femur) relative to the upper portion of the upper leg bone (femur).
SIGNS AND SYMPTOMS:
- With weightbearing the entire extremity appears to be externally positioned. While the child lies on their back the outside of the leg appears to be touching the bed they are lying on. The outside of the foot (small toe side) lies flat on the bed. While the child starts to cruise or stand the child appears unsteady or imbalanced due to a diminished base of support.
- Usually will be a late walker.
- Usually associated with flatfeet.
- Due to the significant external foot progression angle (foot pointing extremely to the outside) a flatfoot develops or worsens as the child is walking through the arch and not over the ball of the foot.
- Extreme poor push off power.
- Runs very poorly.
- Fatigues prematurely with any type of activity.
- Poor overall balance.
- Lacks a desire to participate in sports or any type of activity.
- Associated with poor coordination.
CLINICAL EXAMINATION:
- Examination of the child off weightbearing laying in the supine (on their back) position reveals limited motion of the entire leg going internal and 80-90+ degrees of motion going externally.
- Usually symmetrical (occurs on both sides).
- If unilateral hip dysplasia must be ruled out.
- Must examine the lower leg to rule out external tibial torsion (external position of the lower leg on the upper leg bone) or other associated causes of out toe.
TREATMENT:
- Treatment of femoral retroversion can become very difficult. The primary treatment is to attempt to stretch the muscle group in the hip to improve internal rotation. This must be done aggressively at a very early age to try to improve the overall muscle balance in the hip.
- Avoiding having the child sleep on their stomach with the knees pointed out, which will perpetuate the deformity.
- Splinting of the legs, especially at night to stretch the external rotators and take stress off the internal rotators.
- Exercises to help improve strength to the adductor muscles on the inner upper leg.
- A custom molded orthotic for the shoe at a very early age to prevent the foot from breaking down even further and to provide support necessary for ambulation.
- Getting a child into a sneaker at an early age will help to improve balance when the child starts to walk.
- Assessing for external tibial torsion that may significantly complicate femoral retroversion.
- It may be necessary to place the leg in a cast to stretch the ligamentous and muscular structures on the outside of the knee, which can hold the lower leg externally positioned relative to the upper leg.
PROGNOSIS:
Prognosis is generally poor for femoral retroversion. The child may be
more limited due to a lack of coordination and poor push off strength during
any type of activity. Contractures of the lower leg relative to the
upper leg (external tibial torsion) should be addressed if present to lessen
the deformity. An orthotic may also provide some benefit.
If the condition is causing significant problems and cosmesis is a concern
surgery can be contemplated. If associated with significant external
tibial torsion a lower tibial osteotomy (cutting the lower leg bone and
twisting it in) would provide some benefit. Long-term studies are few
in determining the best treatment outcome for this problem. It is best
to address as much of the deformity as possible (orthotic for foot, casting
for external tibial torsion and stretching exercises to improve the overall
leg position).
Long-term this condition may be associated with hip problems including
arthritis. In a young teenager with hip pain slipped hip growth plates
(slipped capital femoral epiphysis) must be ruled out.
B.
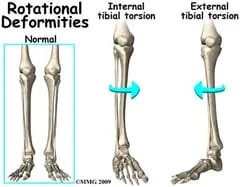
EXTERNAL TIBIAL TORSION
External tibial torsion is usually a common cause of an out toe gait.
The lower leg bone (tibia) rotates excessively to the outside when comparing
it to the upper leg bone (femur).
CAUSE:
- Hereditary.
- Not usually due to in utero position as the fetus’ tibia is usually rotated internal.
- Tight ligament and tendon structures (hamstrings, iliotibial band).
- Can be caused by a true twist of the lower portion of the lower leg bone (tibia) relative to the upper portion of the lower leg bone (tibia).
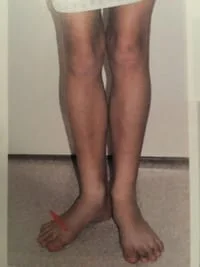
SIGNS AND SYMPTOMS.
- Commonly seen when children begin to walk. Becomes more apparent between the ages of 4 and 7.
- If the hip is normal the knee appears to be straight when watching the child walk but yet the foot and lower leg turn to the outside.
- Usually associated with a flatfoot deformity.
- Poor push off power during running.
- Child may lack coordination during activity.
- Premature fatigue with activity.
- Runs poorly as the child runs through the midfoot and not over the ball of the foot as in a normal gait.
- Usually more commonly seen in one leg more than the other.
- Can be associated with knee Pain (patellofemoral instability).
CLINICAL EXAMINATION:
- With the knee flexed at 90 degrees the lower leg bone (tibia) is rotated in and out relative to the upper leg bone (femur).
- The tibia will rotate excessively towards the outside of the body and very little rotation will go towards the inside.
- Must also examine the hips for femoral retroversion (upper leg bone rotates excessively out with limited motion turning in).
- Must rule out flatfoot deformity which would be made worse by the lower leg position (external tibial torsion).
X-RAYS:
- If the deformity is significant x-rays may be taken. The lower leg bone (transmalleolar axis) is measured relative to the upper leg bone (bicondylar axis of proximal tibia). In an adult it is approximately 14 degrees external.
TREATMENT:
- Full lower extremity examination to rule out other coexisting problems.
- If the foot is flat orthotics are necessary for the foot to prevent the creation of or worsening of a flatfoot deformity. It will also help to bring the foot slightly up and in, lessening some of the appearance of the deformity.
- If associated with excessively tight ligaments and tendons around the knee a short course of immobilization in a cast above the knee may be of some benefit. When a cast is applied the lower leg bone (tibia) is gently rotated internally relative to the upper leg bone (femur). This causes a gentle stretch on the ligament and tendon structures around the knee area. Cast may be necessary for up to 8 weeks depending on the degree of problem.
- Following cast removal night splinting of the leg to hold the lower leg (tibia) in internal rotation relative to the upper leg (femur) may be of some benefit.
- If the condition causes problems with gait, pain in the knee or is of significant cosmetic concern, surgery can be performed at the lower leg (above the ankle growth plate) to take some of the rotation out of the lower leg bone (tibia). Surgery should not be performed until the child is 10 or older.
C.
FLATFOOT DEFORMITY
Flatfeet in children is a common cause of out toe gait, although not readily
appreciated by the general medical community. When the foot points to
the outside (out toe) in hips examination (again, femoral anteversion) and
leg examination (external tibial torsion) has been ruled out then the
primary cause of an out toe gait on a child is a flatfoot deformity.
Some of these deformities occur at the same time. With instability to
the medial arch area the foot flattens and rotates to the outside. In
addition, the arch may appear to be relatively normal but the front part of
the foot is positioned excessively to the outside, relative to the back part
of the foot.
CAUSES:
- Loose or weak ligaments of the arch are the most common reason.
- Bone abnormalities that may be hereditary or acquired from injury (tarsal coalitions or fractures).
- Trauma to tendons and ligaments on the inside of the arch and ankle may cause the arch to slowly or acutely drop.
SYMPTOMS:
- Pain in the arch, feet, ankles and legs aggravated by standing, walking and running.
- Leg cramps and pain at times during the night. Very common in children.
- Premature fatigue during activity or simple walking.
- Weakness in the legs during running.
- Back pain is commonly associated with it.
- Lack of interest in participating in sports or activities that require running.
SIGNS:
- Flat arch when standing is most common. The arch may look normal off weightbearing.
- Many arches appear normal when standing but the front part of the foot points out compared to the rearfoot. This is a foot that functions like a flat foot and may be a problem.
- When looking at the feet from behind the heel bone appears to turn out.
- Knock-knees.
- Feet and ankles look abnormal. Bulging of the bone on the inside of ankle and foot.
- Abnormal gait with the feet excessively turned out.
- Abnormal shoe wear.
RELATED PROBLEMS:
- Development of bunions, hammertoes, heel spurs, neuromas and sagging joints.
- Knee and leg problems.
- Severe collapse of the foot necessitating reconstructive bone surgery.
- Limited activity causing weight gain and poor cardiovascular fitness.
- Muscular tightness in the foot, legs and back.
- Osteoarthritis in the foot, ankle, knees, hips and back.
- Back pain, especially in men over 30.
TREATMENT:
- History and physical examination to identify areas of pain and underlying causes.
- Proper shoe gear to support the foot.
- Orthotics (insoles) custom molded to the foot to support the foot and entire extremity.
- Physical therapy to strengthen weak muscles and stretch tight muscles.
- Short period of cast immobilization to stretch excessively tight muscles that may be aggravating the condition.
Surgery if all efforts at conservative care have failed to alleviate a person’s problem. Failure to consider a surgical alternative may condemn a child or adult with severe deformity to a future of pain, suffering and poor health.
**********
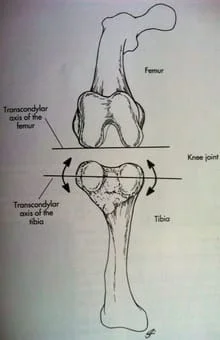
The illustration below depicts the relationship between the femur (thigh bone) and tibia (the larger of the two leg bones) at the level of the knee joint where any abnormal internal or external rotation will cause torsion of the tibia leading to compensation at the ankle and foot with activities.